Categories
Change Password!
Reset Password!


A low-fat diet is associated with a reduction in fatigue in individuals suffering from multiple sclerosis.
According to the findings of a study published in "Multiple Sclerosis Journal", people with multiple sclerosis experienced a notable decrease in fatigue through the implementation of a low-fat dietary intervention. Emma Chase et al. sought to investigate the impact of a low-fat diet on fatigue in multiple sclerosis. A 16-week randomized controlled trial was executed, assigning volunteers with multiple sclerosis (n= 39) to either a low-fat diet group (active [n= 20], with total daily fat calories not >20%) or a wait-list group (control [n= 19]).
The participants underwent a 2-week baseline diet data collection phase using 24-hour diet recalls (24HDRs), after randomization. Subjects in the active group were given 2 weeks of nutrition counseling and then underwent a 12-week intervention with a low-fat diet. Baseline and week 16 data were gathered through a set of three 24HDRs. Every 4 weeks, modified fatigue impact scale (MFIS) and food frequency questionnaire (FFQ) were given. Meanwhile, the people in the control group maintained their pre-study diet and were given diet training upon the completion of the study.
Analysis of 24HDRs revealed no significant difference in total caloric intake between the active and control groups (active: −348 kcal and control: −333 kcal). The active group showed a 10% decrease in fat calories, a 9.0% increase in carbohydrate calories, and an 8.2 grams rise in total fiber intake. Protein calories remained unchanged. The analysis based on the per-protocol (PP) approach revealed a significant reduction in the overall daily intake of fat calories, declining from 39% to 29%, accompanied by a rise in daily carbohydrate calories from 43% to 54% within the active group.
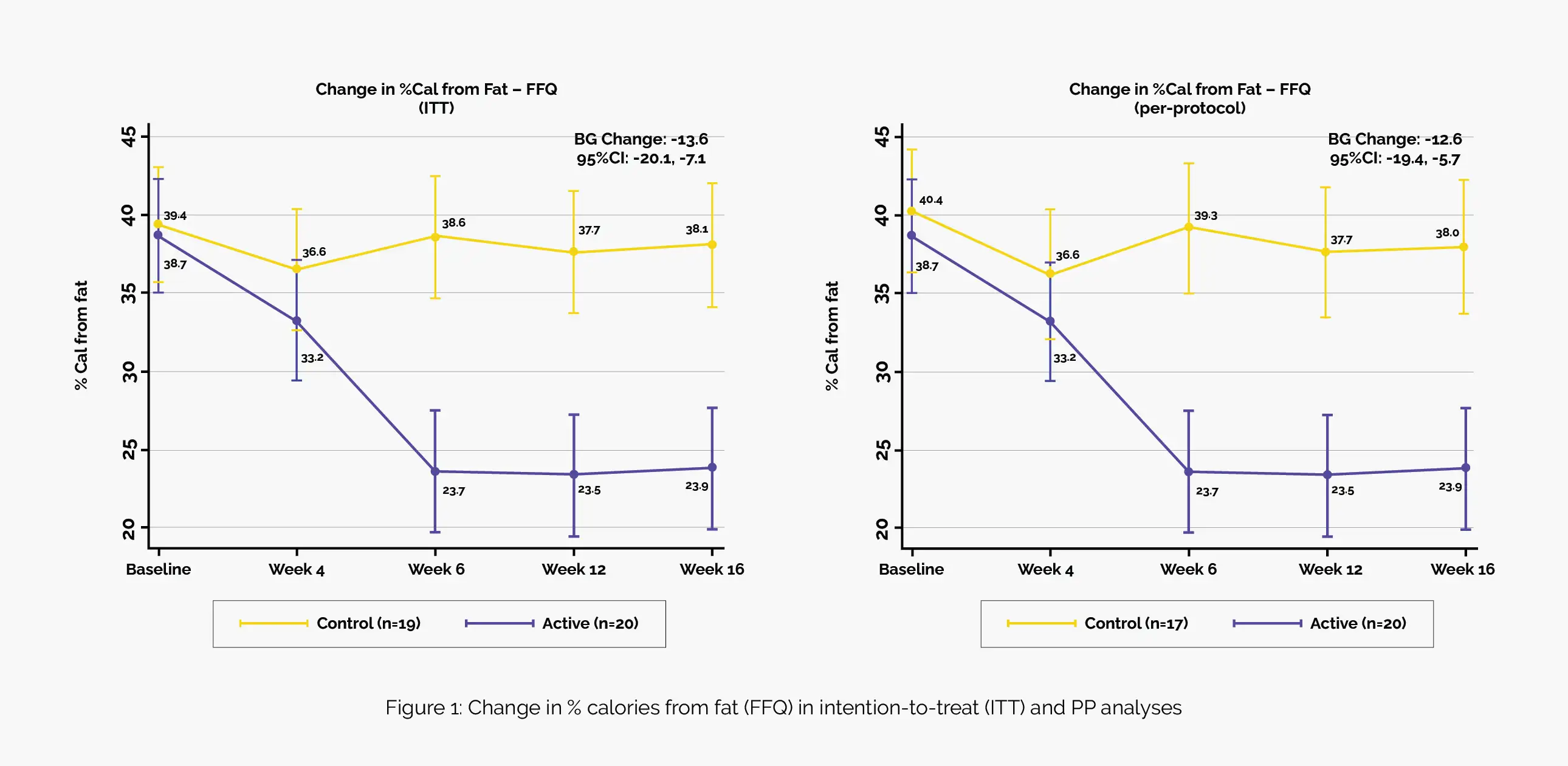
The active group demonstrated a substantial reduction in mean fat calorie intake from 39% at baseline to 24% at the study end, with notable proportions achieving <25% (45%) and <20% (25%) calories from fat. In contrast, the control group showed less adherence, with only 5.3% achieving <25% and 5.3% achieving <20% calories from fat. Overall, the active group displayed a 15% decrease in mean fat calorie intake, significantly more than the 1% decrease observed in the control group (between-group [BG] change = −14), indicating robust adherence to the study diet (Figure 1).
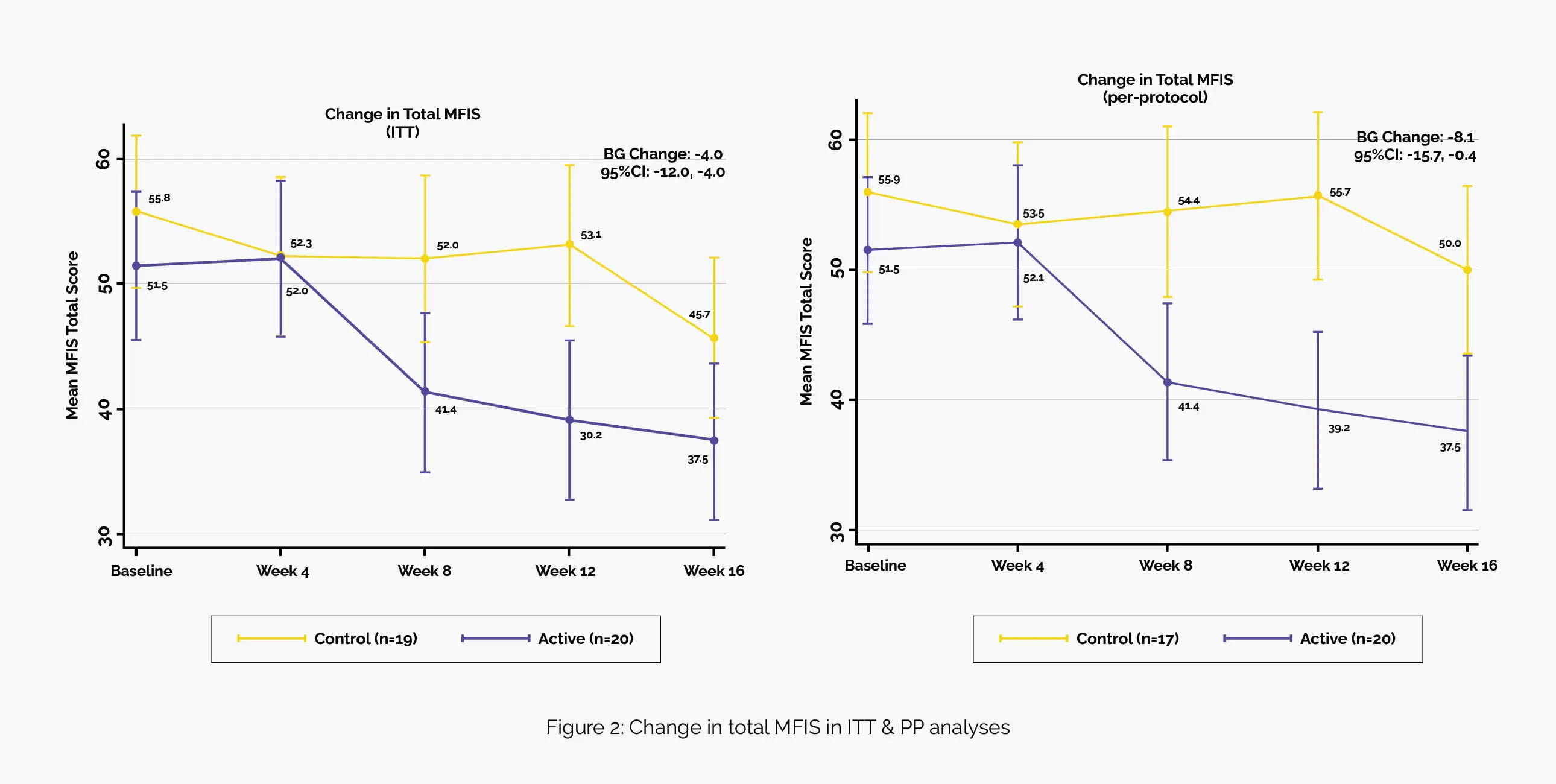
During the ITT analysis, the active group demonstrated a noteworthy mean reduction of 14 points in the total MFIS score, while the control group experienced a reduction of 10 points. The BG mean decrease was 4 points. The PP analysis supported these findings, revealing a BG mean decrease of 8 points, and sensitivity analysis added robustness to this BG decrease by showing a further reduction of 14 points (Figure 2).
Baseline fatigue severity scale (FSS) score was reported to be 6 (±1). In ITT analysis, the active group reduced FSS scores by 0.8 points vs. the control's 0.4 points (BG mean decrease = 0.4 points). In the PP analysis, there was a BG mean decrease of 0.7 points while in the sensitivity analysis, there was a BG mean decrease of 1.2 points. The mean rapid physical activity (RAPA) score rose by 0.3 points among participants in the active group, whereas it declined by 0.6 points in the control group, resulting in a net increase of 0.9 points.
Both groups experienced weight loss (active: 2.4 kg, control: 3.0 kg). In the PP analysis, the weight loss in the control group was adjusted to 1.4 kg and further reduced to 0.9 kg in sensitivity analysis. In contrast, the weight loss in the active group remained consistent. Additionally, the active group exhibited a more substantial within-group change in fat mass compared to lean mass. The active group also demonstrated decreased mean total cholesterol (−12.9 mg/dL) compared to the control's increase (+7.1 mg/dL) (BG difference - 20.0 mg/dL).
Mean low-density lipoprotein cholesterol decreased in the active group (−12.2 mg/dL), while the control arm showed an increase (+6.4 mg/dL) [BG difference - 18.6 mg/dL. High-density lipoprotein cholesterol and mean HbA1c remained unchanged. There was no observed correlation between alterations in MFIS scores and fat calories from the FFQ between baseline and week 16. No safety issues were found in lab assessments. Hence, low-fat dietary intervention (characterized by a substantial increase in carbohydrates and fiber calories and decrease in saturated fat), appears to be a potentially beneficial strategy for symptom alleviation in multiple sclerosis.
Multiple Sclerosis Journal
A low-fat diet improves fatigue in multiple sclerosis: Results from a randomized controlled trial
Emma Chase et al.
Comments (0)