Categories
Change Password!
Reset Password!


A new consensus-based algorithm offers a structured approach for diagnosing and managing functional dyspepsia, with itopride identified as the preferred prokinetic option. The algorithm emphasizes tailored therapies, including acid-suppressing treatments and neuromodulators, to improve patient outcomes.
Functional dyspepsia (FD), a condition involving gut-brain interaction, causes symptoms such as epigastric pain, bloating, early satiety, and nausea. It affects 11–30% of the global population and substantially impedes quality of life. The diagnostic challenges associated with FD highlight the need for clear, tailored guidelines.
To address these challenges, 50 gastroenterologists participated in focus-group discussions to develop a consensus-based algorithm for FD care. The discussions focused on key aspects, including history-taking, recognizing alarm symptoms, endoscopic evaluations, H. pylori testing and eradication therapy.
Diagnosis
FD is diagnosed based on characteristic symptoms, medical history, and the exclusion of other upper gastrointestinal (GI) or abdominal conditions. A thorough history and clinical examination are imperative to rule out conditions such as peptic ulcer, cancers, thyroid disorders, and renal issues, especially in those over 45 or those with alarm symptoms like weight loss or dysphagia.
Investigation typically involves upper GI tract endoscopy to exclude organic causes, including H. pylori infection, and may encompass additional lab tests (e.g., complete blood count, liver and thyroid function tests) and abdominal ultrasonography. For people with alarm features or those unresponsive to previous treatment, endoscopy is critical. H. pylori eradication is suggested, especially in regions with high gastric cancer rates, and persistent symptoms after eradication may indicate FD.
Additional diagnostic tests, such as plain abdominal X-ray, gastric scintigraphy, electrogastrography (EGG), computed tomography scan, celiac serology (in regions with high celiac disease prevalence), and endoscopic deep duodenal biopsies, can help confirm the diagnosis of FD or exclude other underlying causes of chronic dyspeptic symptoms.
Treatment
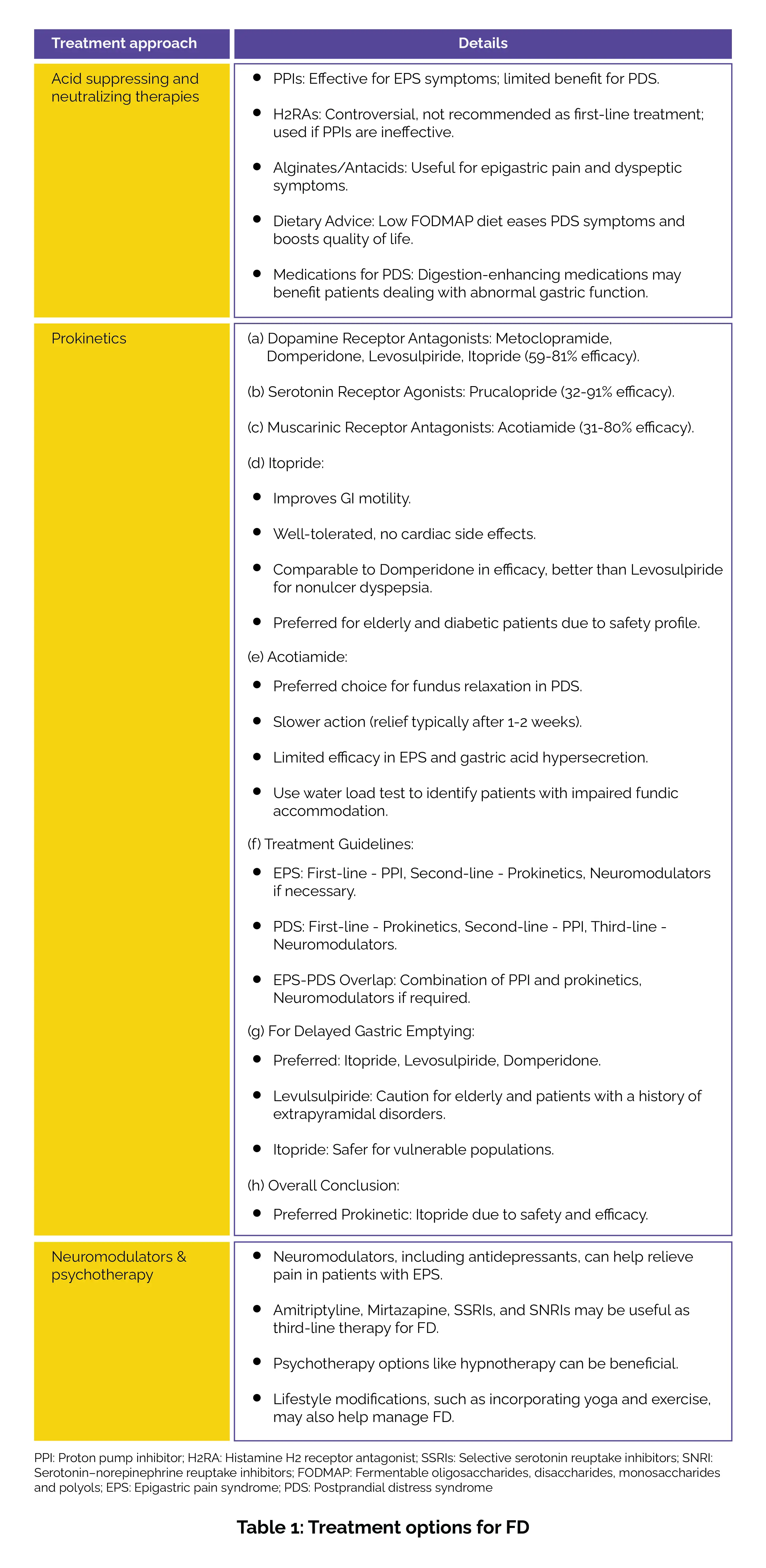
Managing FD involves a combination of acid-suppressing therapies, prokinetics, and neuromodulators tailored to the specific subtype. Proton pump inhibitors (PPIs) are effective for the epigastric pain syndrome (EPS) subtype, while prokinetics like itopride are preferred for postprandial distress syndrome (PDS). Neuromodulators and psychotherapy, such as selective serotonin reuptake inhibitors (SSRIs) and hypnotherapy, may be considered for refractory cases, where first-line treatments are ineffective. Treatment should be reassessed after 4-6 weeks to adjust therapy based on patient response. Table 1 summarizes various treatment modalities for FD.
Algorithm
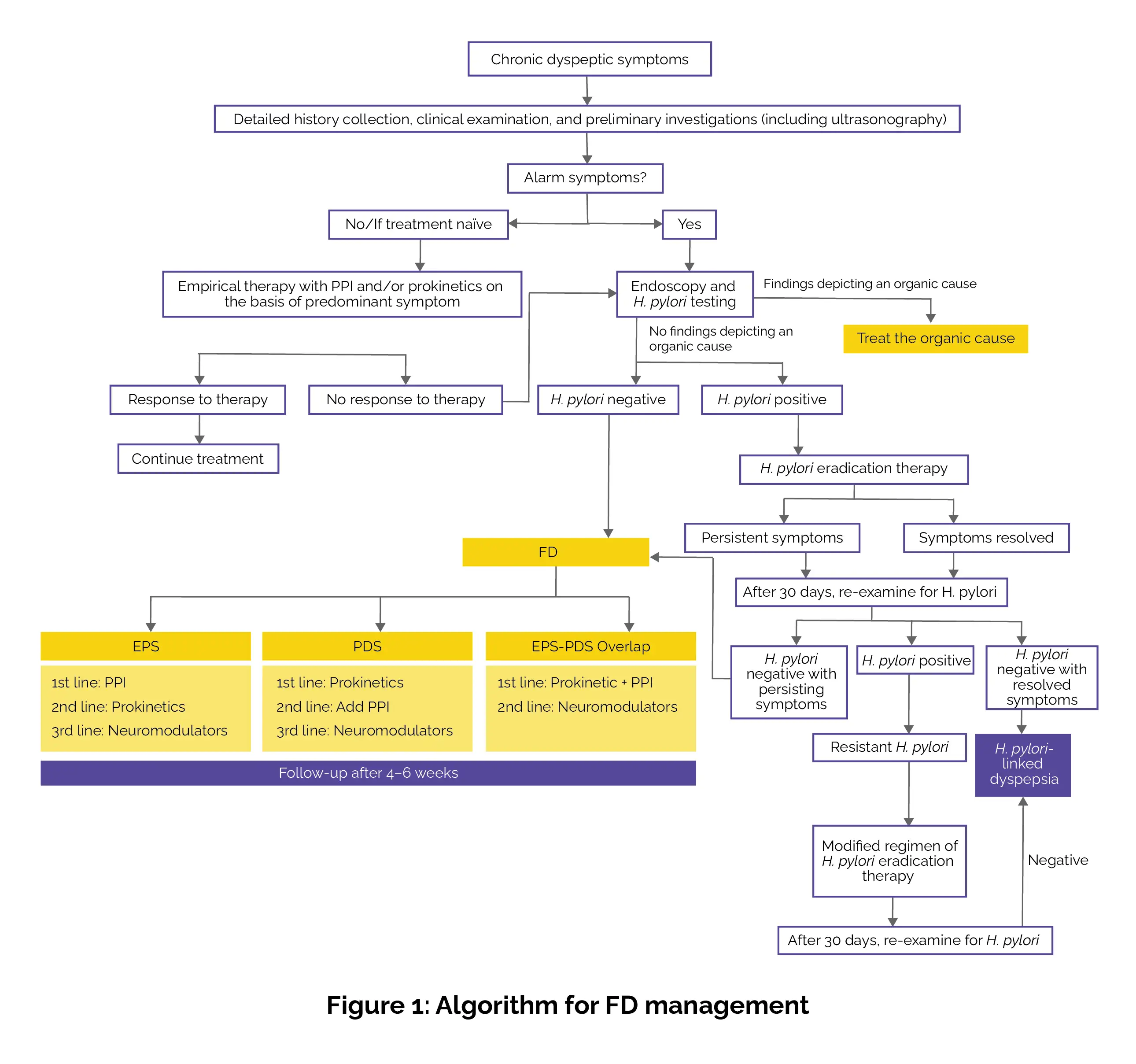
The expert-developed algorithm emphasized a stepwise approach to treatment, starting with a comprehensive patient evaluation and the identification of alarm symptoms. Based on symptoms or FD subtype—EPS, PDS, or the EPS-PDS overlap—treatment is tailored (Figure 1).
This new approach offers a structured, evidence-based framework for clinicians to tackle FD more effectively, ultimately reducing the burden of this common GI disorder.
Journal of The Association of Physicians of India
Proposed Algorithm for the Diagnosis and Management of Functional Dyspepsia in India
Showkat A Zargar et al.
Comments (0)