Categories
Change Password!
Reset Password!


The updated guidelines and evolving landscape of pain management emphasize the growing importance of interventional treatments like pulsed radiofrequency, offering new hope for patients battling severe herpes zoster-related pain.
Managing the pain associated with acute herpes zoster (HZ) and postherpetic neuralgia (PHN) remains a significant challenge for both patients and healthcare providers. This review in ‘PAIN Practice’ updated the previous guideline published in 2011 and revised in 2015 (published in 2019), highlighting both conventional and new interventional approaches that show promise in offering relief for those struggling with persistent post-infection pain. Among these, pulsed radiofrequency (PRF) of the dorsal root ganglion stands out as a potential breakthrough.
PHN, which causes chronic, debilitating pain in one or more dermatomes following an HZ infection, affects approximately 1 in 4 people who suffer from acute HZ, affecting the quality of life. Acute HZ itself occurs in about 3 to 5 individuals per 1,000 person-years, and for many, this pain transitions into PHN, resisting conventional treatments.
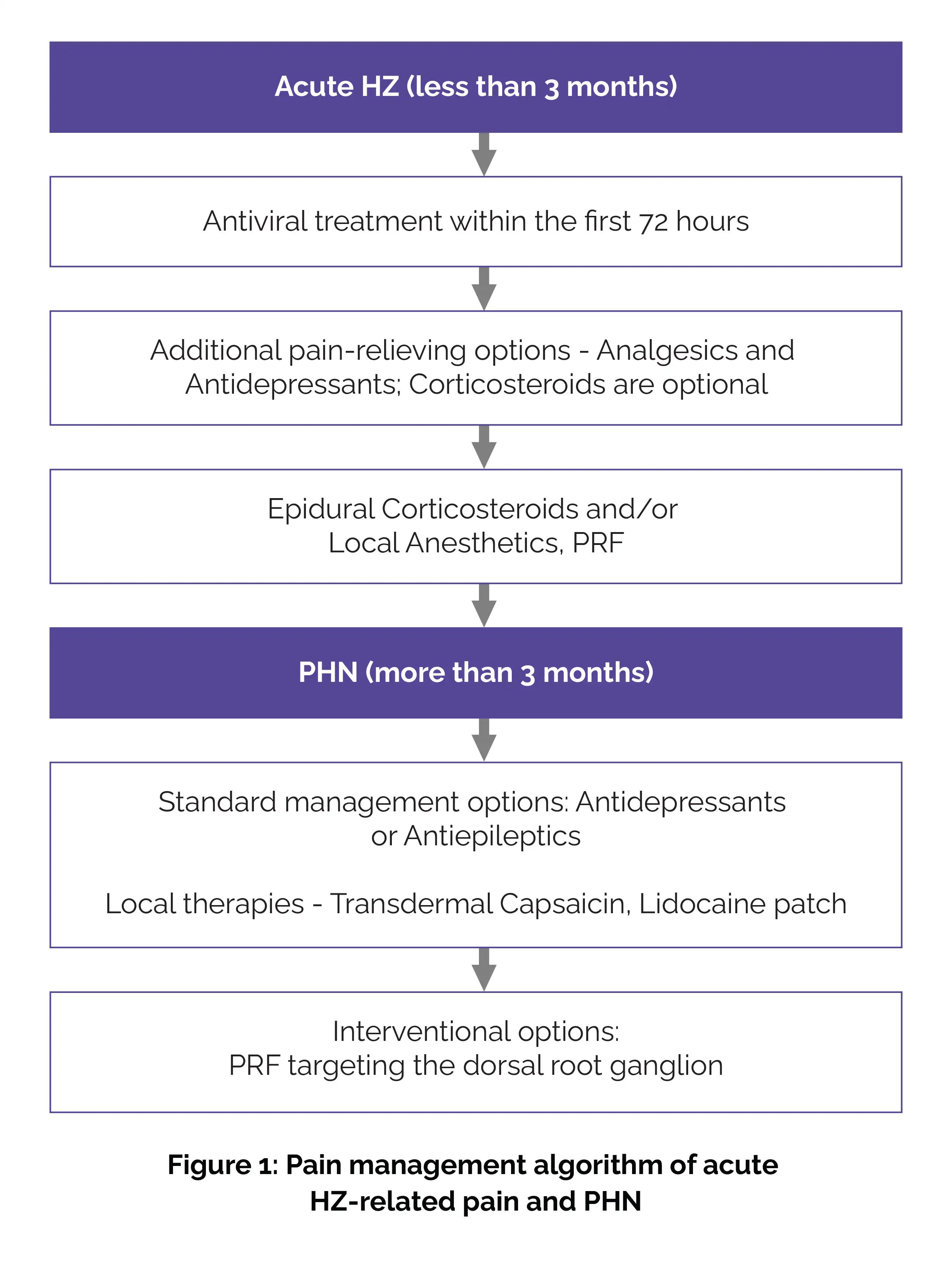
Current treatment strategies emphasize antiviral therapy, ideally started within 72 hours of symptom onset to address the initial pain. Symptomatic treatments, such as analgesics, tricyclic antidepressants (like nortriptyline), and antiepileptic medications (like gabapentin), are also crucial for pain management.
However, when pain persists, interventional options become necessary. Epidural injections with local anesthetics and corticosteroids are one approach, but PRF targeting the dorsal root ganglion has emerged as the most promising method for reducing pain in PHN patients. For PHN specifically, transdermal capsaicin, lidocaine, and oral medications (e.g., antidepressants or antiepileptics) are often recommended treatment options (Figure 1):
Yet, the high failure rates of traditional therapies underline the crucial need for pioneering solutions.
PAIN Practice
Herpes zoster and post herpetic neuralgia
Elisabeth J. M. Adriaansen et al.
Comments (0)