Categories
Change Password!
Reset Password!


For treatment-resistant depression, Stanford neuromodulation therapy is superior to sham stimulation.
In a double-blind randomized controlled trial, Stanford neuromodulation therapy (SNT, an accelerated, high-dose, patterned, functional connectivity magnetic resonance imaging [fcMRI]-guided intermittent theta-burst stimulation [iTBS] protocol) substantially reduced depression symptoms following five days of intervention compared to an equivalent course of sham stimulation in a treatment-resistant sample. Eleanor J. Cole et al. sought to examine the antidepressant effectiveness of SNT for treatment-resistant depression.
Subjects having treatment-resistant depression who were undergoing moderate-to-severe depressive episodes were randomly allocated to get active or sham SNT. The area of the left dorsolateral prefrontal cortex that is most functionally anti-correlated with the subgenual anterior cingulate cortex was specifically targeted using resting-state functional MRI. Assessment of the Montgomery- Åsberg Depression Rating Scale (MADRS) score four weeks following therapy was the major endpoint.
Overall, 32 subjects with treatment-resistant depression had been recruited at the time of the planned interim analysis, and 29 volunteers who continued to meet the requirements for inclusion got either active (n = 14) or sham (n = 15) SNT. In the active treatment group, the mean percent reduction in MADRS score from baseline at 4 weeks after treatment was greater when compared to the sham treatment group, as shown in Table 1:
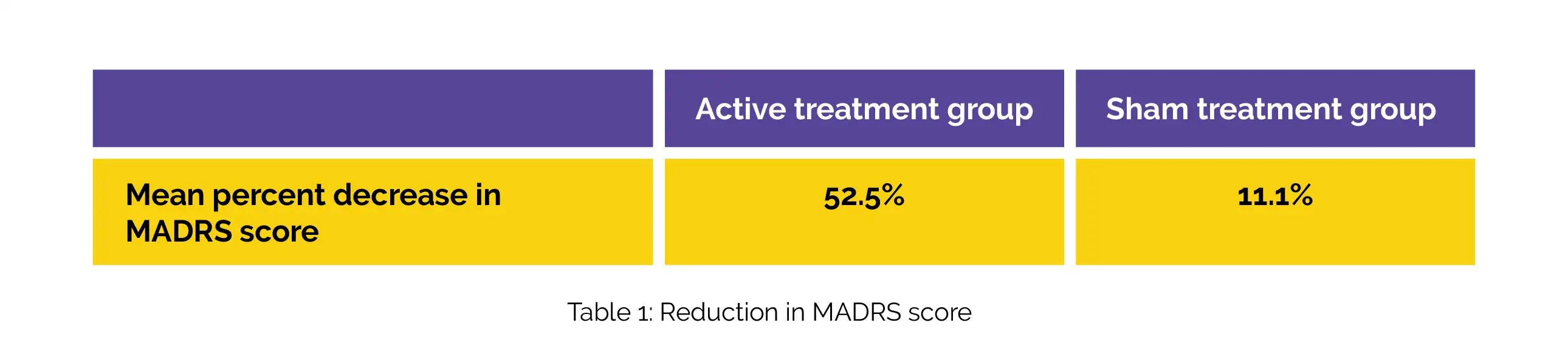
SNT outperformed sham stimulation to relieve treatment-resistant depression. During the study, no severe adverse events took place. Due to SNT's short duration and high antidepressant efficacy, it offers a chance to treat patients in emergency or inpatient settings, where a compressed time course is required. To ascertain SNT's durability and to contrast it with alternative therapies, more trials should be conducted.
The American Journal of Psychiatry
Stanford Neuromodulation Therapy (SNT): A Double-Blind Randomized Controlled Trial
Eleanor J. Cole et al.
Comments (0)